The Nu Guide to Anatomy 101
How we understand our own genital anatomy, the words we use and how we perceive our internal and external construct is very important when it comes to understanding how our bodies work and what to do when things change.
When seeking advice for vulvovaginal symptoms, typically with your GP, or with a gynaecologist or women’s health physiotherapist, it is crucial that you are familiar with the correct anatomical terms so that you can speak the same language as your health provider and help them to understand exactly where you are experiencing symptoms.
There is no longer a place for euphemistic language.
To keep it simple, there are two key words that you need to use precisely:
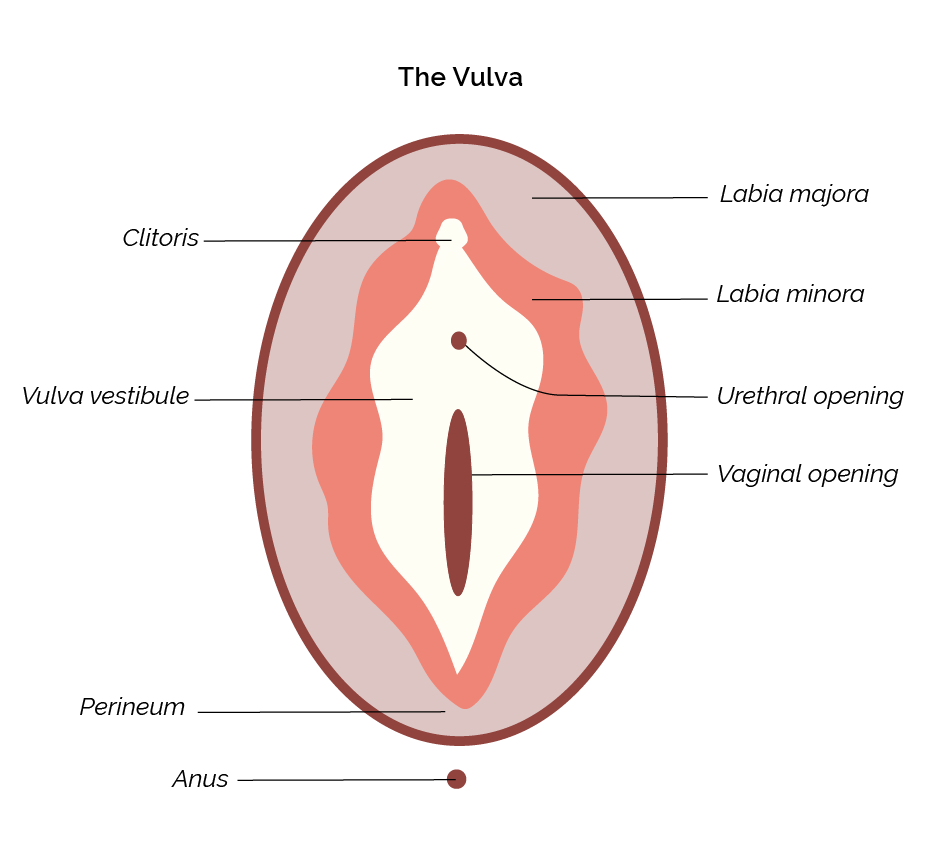
Vulva - this is the external genital region and includes the hair-bearing mons pubis, inner and outer labia, through to the vaginal opening.
Vagina - this is the tubular muscular passage which connects the vulva to the cervix. It is made up of elastic skin with a good blood supply and is supported by the pelvic floor muscles.
It can be difficult to accurately locate where a sensation is occurring. Pay attention when you are experiencing symptoms so that you can give a detailed road map. Use a mirror or take a selfie with your phone. Notice which areas of skin are affected and if there is any change in appearance and when the sensations are more intense. Health providers aren’t mind readers - if you tell them that you are experiencing pain in your vagina when it’s actually in the clitoris or labia they will be heading off in the wrong direction!
Consulting your health professional.
It’s good practice for your doctor to perform an examination to evaluate your symptoms. You can bring a support person along to your appointment or ask for a nurse chaperone to come in while the doctor examines you. You are always able to decline an examination or defer it to a subsequent visit if you feel more comfortable. This should not affect the standard of care you receive but may delay the timeframe to diagnosis.
Above all, it’s OK to be OK with the anatomy of your body. Being aware of what you feel when things are good - and when they are not - will help you develop a closer relationship to your own body and to your own sense of comfort, discomfort and even pleasure.